Bowen et al. Autologous hematopoietic cell transplantation following high-dose immunosuppressive therapy for advanced multiple sclerosis: long-term results. Bone Marrow Transplant. 2011 [Epub]
The purpose of the study was to determine the long-term safety and effectiveness of high-dose immunosuppressive therapy (HDIT) followed by autologous hematopoietic cell transplantation (AHCT) in advanced multiple sclerosis (MS).
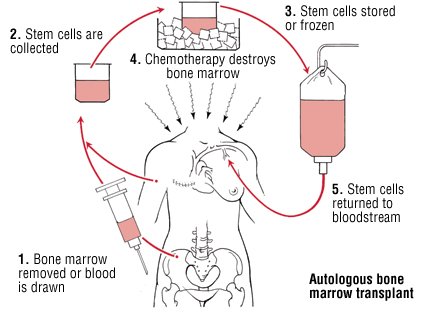
Methods: Total body irradiation, cyclophosphamide and anti-thymocyte globulin(to kill T cells) were followed by transplantation of autologous, CD34-selected peripheral blood stem cells. Neurological examinations, brain magnetic resonance imaging and cerebrospinal fluid (CSF) for oligoclonal bands (OCB) were serially evaluated. Patients (n=26, mean Expanded Disability Status Scale (EDSS)=7.0, 17 secondary progressive, 8 primary progressive, 1 relapsing/remitting) were followed for a median of 48 months after HDIT followed by AHCT.
Results: The 72-month probability of worsening 1.0 EDSS point was 0.52 (95% confidence interval, 0.30-0.75). Five patients had an EDSS at baseline of 6.0; four of them had not failed treatment at last study visit. OCB in CSF persisted with minor changes in the banding pattern. Four new or enhancing lesions were seen on MRI, all within 13 months of treatment. In this population with high baseline EDSS, a significant proportion of patients with advanced MS remained stable for as long as 7 years after transplant. Non-inflammatory events may have contributed to neurological worsening after treatment.
Conclusions: HDIT/AHCT may be more effective in patients with less advanced relapsing/remitting MS.
"Impressive results, pity the short-term risks associated with bone marrow transplantation are so high. In some registries the risk of dying from a complication of bone marrow transplantation is ~5%. Are you prepared to take these risk?"