Bone marrow transplantations seems to get rid of autoimmune cells in MSers. #MSBlog #MSResearch
"This is a study for immunology geeks. In short MSers who have autologous bone marrow transplantation (BMT), i.e. their immune systems are rebooted using their own stem cells, have evidence to support that the type of immune cells that come back after the transplant are not autoreactive These results support the concept of rebooting the immune system to treat autoimmunity. Interestingly, in MSers on natalizumab these cells are still present and are prevented to get into the brain and spinal. This is why MS comes back with a vengeance when natalizumab is stopped. Natalizumab is like sticky plaster or band aid; remove the sticky plaster and the disease is back. BMT and other induction or rebooting therapies get to the core of the problem; i.e. they attempt to cure autoimmunity. You have to realise, however, that BMT will not be effective in all people treated. When the immune system is ablated some autoreactive cells may survive and come back when the immune system reconstitutes itself. "
"Would you have a bone marrow transplant (BMT)? The risks associated with it are very high; it has a mortality (chance of dying from the procedure) approaching 5%. Although in the best BMT units this figure is below 1%. I personally think treatment with alemtuzumab is preferable; it probably achieves a similar result with less risk of death. Alemtuzumab, however, does have its own risks of other types of autoimmunity developing when the immune system recovers."
Background: Autologous hematopoietic stem cell transplantation (HSCT) for relapsing-remitting multiple sclerosis is a potentially curative treatment, which can give rise to long-term disease remission. However, the mode of action is not yet fully understood.
Objective: The aim of the study was to evaluate similarities and differences of the CD4+ T cell populations between HSCT-treated MSers (n=12) and healthy controls (n=9).
Methods: The investigators' performed phenotyping of memory T cells, Tregs, T helper type 1 (Th1) and T helper type 17 (Th17) cells. Further, T cell reactivity to a tentative antigen: myelin oligodendrocyte glycoprotein was investigated in these MSer populations. MSers treated with natalizumab (n=15) were included as a comparative group. White blood cells were analyzed with flow cytometry and T cell culture supernatants were analyzed with magnetic bead panel immunoassays.
Results: HSCT-treated MSers had similar levels of Tregs, Th1 and Th17 cells as healthy subjects, whereas natalizumab-treated MSers had lower frequencies of Tregs, and higher frequencies of Th1 and Th17 cells. Cells from HSCT-treated MSers cultured with overlapping peptides from myelin oligodendrocyte glycoprotein produced more TGF-β1 than natalizumab-treated MSers suggestive of a suppressive response. Conversely, T cells from natalizumab-treated MSers cultured with those peptides produced more IL-17, IL-1 and IL-10 indicating a Th17 response.
Conclusion: In conclusion, they demonstrate circumstantial evidence for the removal of auto-reactive T cell clones as well as development of tolerance after HSCT. These results parallel the long-term disease remission seen post HSCT.
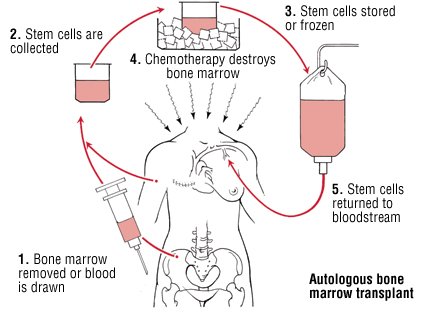
"The following picture explains the steps involved in performing an autologous BMT. After step 4 the immune system is very suppressed and the person needs bone marrow support; transfusions for anaemia and low platelets for bleeding and antibiotics to prevent or treat infections. The infections can be very serious and life threatening."