Firstly, here is the wikepedia version [click].
And now mine - as clinicians when we say there's spasticity in an arm/leg we mean that there's increased resistance to movement of the arm/leg at the level of it's joint. For example, this is the knee joint for the lower leg, or the hip for the upper leg.
This happens due to increased muscle tone (termed a high tone/hypertonus) and varies with the speed of movement at the joint. This is opposed to rigidity which is present throughout the range of movement, and is seen in conditions such as Parkinson's disease.
Spasticity can be mild with simply a catch on bending and extending the leg at the knee joint or severe where the leg may remain in a flexed posture even at rest and lead to contractures (permanent shortening of the muscle) and painful spasms. Spinal cord lesions as opposed to brain lesions tend to have more spasticity than brain lesions.
Spasticity often does not occur in isolation and is commonly seen together with:
- Abnormal reflex transmission with increased gain on reflexes
- Clonus (muscle spasm with repeated, rhythmic contractions - on flexing a muscle or simply on movement)
- Painful muscle spasms (which are sudden involuntary [i.e. happen without any planned intention] movements involving multiple muscles in response to movement or touch)
- Dystonia (tonic muscle overactivity without triggers due to an inability of the nerve innervating the muscle to stop firing after voluntary movement or reflex activity)
- Co-contraction (inappropriate activation of the opposing muscles during voluntary movement leading to loss of dexterity and slowed movements)
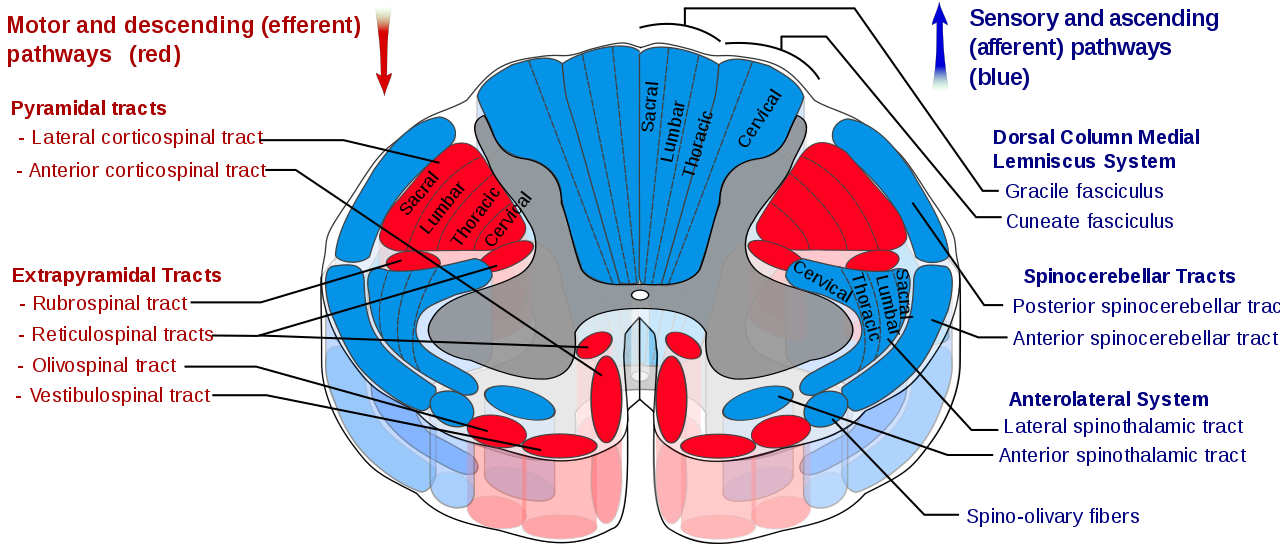
Cross-section through the spinal cord (ascending and descending tracts to and from the brain).
In the spinal cord for sometime the wildly held belief was that spasiticity was caused by damage to the corticospinal tract (all of these pathways except the medial reticulospinal tract and vestibulospinal tract are held under INHIBITORY control by the brain), but it is now understood that other motor tracts may also play a role:
- The lateral reticulospinal tract which is adjacent to the corticospinal tract (see diagram above) may be involved in MS where lesions have a predilection for the lateral surface of spinal cord. This pathway has an inhibitory effect on stretch reflexes.
- The medial reticulospinal tract and vestibulospinal tract (see diagram above) which have excitatory effects on extensor muscle tone.
Whereas lesions affecting the brain leads to increased excitation of the spinal pathways and a lowering of the threshold (i.e. easily triggered) to respond to stimuli such as stretch.
There are certain things which worsen spasticity:
- skin ulcers, ingrown toenails, skin infections
- constipation, UTIs, kidney stones, and pain
- improper seating, ill fitting orthotics
- rapid withdrawal of anti-spasticity medication
- other- deep vein thrombosis/DVT, injuries, stress

 Pharmacological medications commonly used include Baclofen (GABAergic drug which relieves spasms) often in combination with Tizandine (centrally acting alpha2-noradrengic drug) as their mechanism of action is complimetary. Gabapentin is also a useful anti-spasmodic but limited by its sedative side effects, the latter also occurs with Baclofen. Botox is useful when individual muscles are involved. When oral anti-spasticity medications are of limited use, intrathecal Baclofen which delivers Baclofen into the spinal space may be used. Rarely, drastic measures are taken for painful immobile spastic legs with reflex spasms using intrathecal phenol or alcohol which causes irreversible nerve damage. Other measures include relief of pain and discomfort, improvement in posture, stretch exercises, facilitation of sitting, standing and walking, and prevention of complications such as contractures and pressure sores. Contractures which are not severe can be corrected using sequential casting (see below).
Pharmacological medications commonly used include Baclofen (GABAergic drug which relieves spasms) often in combination with Tizandine (centrally acting alpha2-noradrengic drug) as their mechanism of action is complimetary. Gabapentin is also a useful anti-spasmodic but limited by its sedative side effects, the latter also occurs with Baclofen. Botox is useful when individual muscles are involved. When oral anti-spasticity medications are of limited use, intrathecal Baclofen which delivers Baclofen into the spinal space may be used. Rarely, drastic measures are taken for painful immobile spastic legs with reflex spasms using intrathecal phenol or alcohol which causes irreversible nerve damage. Other measures include relief of pain and discomfort, improvement in posture, stretch exercises, facilitation of sitting, standing and walking, and prevention of complications such as contractures and pressure sores. Contractures which are not severe can be corrected using sequential casting (see below).
Stretch exercises (left) and manual sequential casts (right)