Michael Pender, MD, PhD; Peter Csurhes; Corey Smith; Nanette Douglas; Michelle Neller, PhD; Leone Beagley, PhD; Sweera Rehan, PhD; Tracey Hopkins, PhD; Kate Thompson, PhD; Stefan Blum, MD; Kerryn Green, MBBS; Zara Ioannides, MD; Alan Coulthard, PhD; Kaye Hooper, PhD; Scott Burrows, PhD; Rajiv Khanna, PhD
Objective: To determine the safety of treating progressive multiple sclerosis (MS) patients with autologous Epstein–Barr virus (EBV)-specific T cells. Background: Mounting evidence indicates a role for EBV in MS pathogenesis. EBV-infected autoreactive B cells might accumulate in the CNS because of defective cytotoxic CD8+ T-cell immunity.
Design/Methods: In this trial we administer autologous EBV-specific T cells to patients with progressive MS (EDSS 5.0–8.0). Each patient receives their own T cells stimulated ex vivo to enhance reactivity to EBV nuclear antigen-1, latent membrane protein 1 (LMP1) and LMP2A, and is followed through 26 weeks. Four escalating dose infusions are administered biweekly.
Results: To date, four SPMS patients and one PPMS patient have been treated. No significant adverse events have been observed. Three patients experienced symptomatic and objective clinical improvement, which commenced 2–8 weeks after the first infusion and was most marked in the two patients receiving T cells with the highest EBV reactivity. Striking improvement occurred in one SPMS patient, with normalization of lower extremity tone and plantar (Babinski) responses for the first time in 16 years, increased walking distance with walker from 100 metres at baseline and for the previous 5 years to 1200 metres, marked reduction in fatigue, increased manual dexterity, and improvements in lower extremity power, reflexes and sensation. A second SPMS patient had reduced fatigue, increased productivity and improved balance. The third responder (PPMS) had improved colour vision, visual acuity and manual dexterity and reduced fatigue, lower extremity spasms and urinary urgency. These data are consistent with prior data from the first patient ever treated (SPMS compassionate use) who experienced reduced fatigue and lower extremity spasms, and improved cognition, hand function and productivity.
Conclusions: This is the first report of clinical improvement in a prospective trial of autologous EBV-specific T cells to treat progressive MS patients. Further studies are planned.
Study Supported By: Multiple Sclerosis Society of Queensland, Multiple Sclerosis Research Australia and Perpetual Trustee Company Limited
This isa safety study designed to test whether vaccination against EBV could impact on MS. They have made viral reactive CD8 T cells and transfer them in to kill the EBV infected (B) cells. This will be of interest, so maybe ProfG may have time to tweet or report on the presentation.
In the AAN press release it said the trial was designed to look at ten people and have found it should have been five with PPMS and five with SPMS. In the trial, the volunteers received four escalating doses of cytotoxic CD8 T cells over six weeks and were followed for an additional twenty weeks after the last dose.
Here the abstract above it says five people were looked but in the press release from the AAN, it says six. These results are encouraging, but the study is seemingly unblinded and is reporting symptomatic improvements and this is not what a trial in progression may go for. But being a phase I it is designed to say it is safe.
This study used autologous cells, so they were generated from the same people who they were later received the cells back after they were expanded.
However, this data is now being reported as company data. It appears the company has got some rights from the University in Queensland.
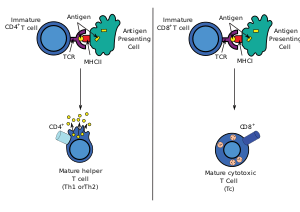
Anyway according to the company website. They are planning to use their product as allogenic cells, i.e. made in one person to be used in another person. Whilst this will help in production of a standardised cell this, without more data on the technology, makes little immunological sense as to get proper engagement of cells you need your antigen presenting cells to present to your own T cells.
An allogenic cell may not recognize the B cells infected with EBV in another person, but they can recognize a large percentage of other peoples major histocompatibility complexes (transplantation antigens) as a target, so you could be injecting cells that that can potential kill every cell in the recipient. I hope not.
More likely the injected cells will last about 5 days and then the recipient will destroy them as being invaders.