I can hear you saying, "Oh no not another B-cell paper!". However, this is where the action is. It is the B-cell and not the T-cell. Do you agree or disagree? Have your say.
Clonal relationships of CSF B cells in treatment-naive multiple sclerosis patients.
Clonal relationships of CSF B cells in treatment-naive multiple sclerosis patients.
Eggers EL, Michel BA, Wu H, Wang SZ, Bevan CJ, Abounasr A, Pierson NS, Bischof A, Kazer M, Leitner E, Greenfield AL, Demuth S, Wilson MR, Henry RG, Cree BA, Hauser SL, von Büdingen HC.
JCI Insight. 2017 Nov 16;2(22). pii: 92724. doi: 10.1172/jci.insight.92724. [Epub ahead of print
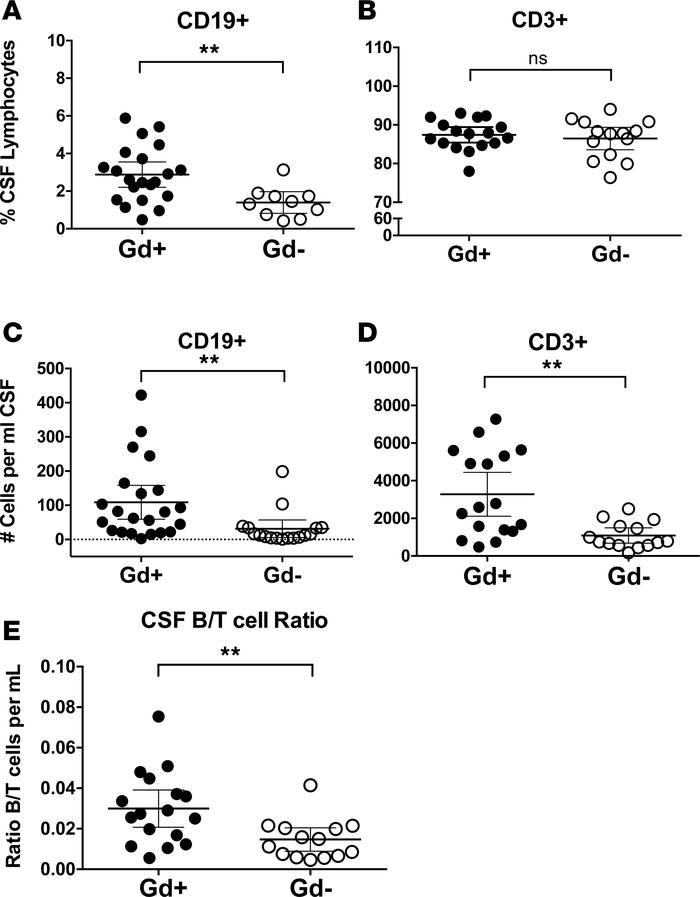
A role of B cells in multiple sclerosis (MS) is well established, but there is limited understanding of their involvement during active disease. Here, we examined cerebrospinal fluid (CSF) and peripheral blood (PB) B cells in treatment-naive patients with MS or high-risk clinically isolated syndrome. Using flow cytometry, we found increased CSF lymphocytes with a disproportionate increase of B cells compared with T cells in patients with gadolinium-enhancing (Gd+) lesions on brain MRI. Ig gene heavy chain variable region (Ig-VH) repertoire sequencing of CSF and PB B cells revealed clonal relationships between intrathecal and peripheral B cell populations, which could be consistent with migration of B cells to and activation in the CNS in active MS. In addition, we found evidence for bystander immigration of B cells from the periphery, which could be supported by a CXCL13 gradient between CSF and blood. Understanding what triggers B cells to migrate and home to the CNS may ultimately aid in the rational selection of therapeutic strategies to limit progression in MS.
In active disease there are more B cells accumulating in the CNS....but what are they?
Yes you guessed it they are B memory Cells.
The population is the Class Switched memory B cell, There were also more plasma cells (did these come from memory cell population).
The finding that increased CSF B cells were linked to the presence of Gadolinium (Gd) lesions on brain MRI suggested their association with disease activity in MS and raised the question whether there are clonal relationships between CSF B cell subsets and their PB counterparts.
Interestingly, they found evidence peripherally antigen-stimulated B cells may have migrated to the CSF compartment where they became activated to further mature into antibody-secreting CD27 high B cells.
They found clonally related CD27hi PCs (plasmablasts/plasma cells) in blood and CSF that were also related to Ig class-switched-memory B cells in the same compartments.
Given that CD27hi PCs are likely restricted to their compartment (as evidenced by their low CXCR5 expression), and the persistence of memory B cells in MS CSF and CNS in general, parallel maturation of preexisting class switched memory B cells on both sides of the blood-brain barrier may have occurred following a peripheral immune activating event.
The presence of clonal relationships between memory B cells and plasma cells in the CSF and CSF Ig-VH clusters containing related IgM-VH and IgG-VH also support local B cell activation and subsequent maturation and class-switch recombination.
They did find naive CSF B cells with clonally related counterparts in the periphery, naive B cells do not seem to become stimulated intrathecally to mature to memory B cells.
So its B memory Cells
Peripheral immune activation can lead to intrathecal immune stimulation, either via antigen nonspecific (