Ann Neurol. 2018 Mar 31. doi: 10.1002/ana.25219. [Epub ahead of print]
Permeability of the blood-brain barrier predicts no evidence of disease activity at two years after natalizumab or fingolimod treatment in relapsing-remitting multiple sclerosis.
Cramer SP, Simonsen HJ, Varatharaj A, Galea I, Frederiksen JL, Larsson HBW.Abstract
OBJECTIVE:
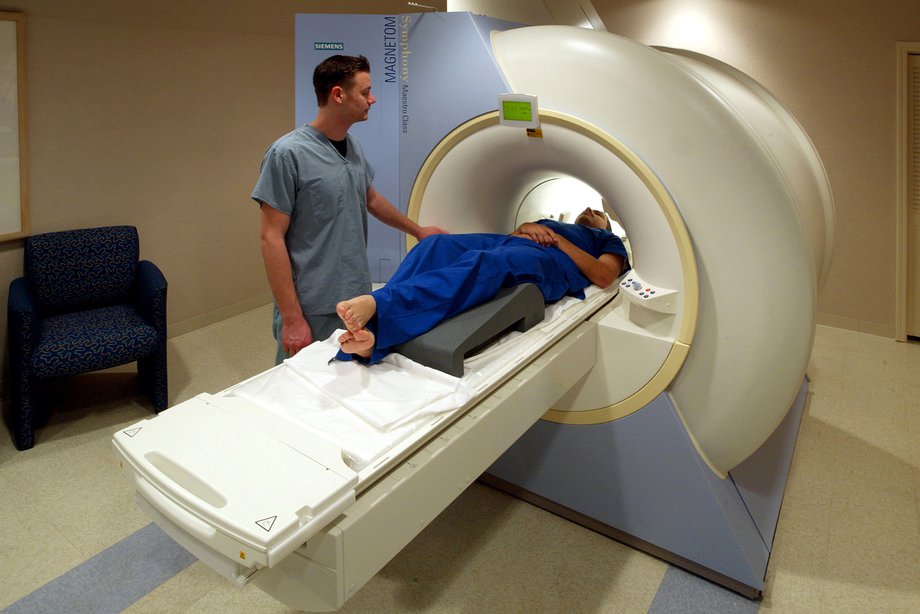
To investigate if blood-brain barrier (BBB) permeability, as measured by dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI), can provide early detection of sub-optimal treatment response in relapsing-remitting multiple sclerosis (RRMS).
METHODS:
35 RRMS patients starting on fingolimod or natalizumab, drugs with a common effect of decreasing lymphocyte influx into the CNS, were scanned with DCE-MRI at 3T prior to treatment and at three and six-months post-treatment. We calculated the influx constant Ki , a measure of BBB permeability, using the Patlak model. Sub-optimal treatment response was defined as loss of no evidence of disease activity (NEDA-3) status after two years of treatment.
RESULTS:
Subjects with loss of NEDA status at 2 years had a 51% higher mean Ki in normal-appearing white matter (NAWM) measured after six months of treatment, compared to subjects with maintained NEDA status (mean difference 0.06 (CI 0.02-0.09) ml/100g/min; p=0.002). Ki in NAWM at 6 months was a good predictor of loss of NEDA status at two years (AUC 0.84, CI 0.70-0.99; p=0.003) and a value above 0.136 ml/100/g/min yielded an odds ratio of 12.4 for sub-optimal treatment response at 2 years, with a sensitivity of 73% and a specificity of 82%.
INTERPRETATION:
Our results suggest that BBB permeability as measured by DCE-MRI reliably predicts sub-optimal treatment response and is a surrogate marker of the state of health of the BBB. We find a predictive threshold for disease activity, which is remarkably identical in clinically isolated syndrome as previously reported and established RRMS as investigated here.
“If you want something new, you have to stop doing something old”
― Peter F. Drucker (Management consultant)
Of course, I'm not talking about a businesses in the literal sense, but believe it or not science is one of the largest de-centralized business offerings in the world. The beauty of it is that it is also very much sustainable. The human race will never tire of the value of the wonder of discovery. Take Tesla, for instance.
But going back to what this article is about, I ask the question, why replace our existing MRI measures of Gadolinium (or contrast enhancement) and number of or expanding T2 lesion load as markers of disease activity in MS? The answer is, until something better comes along. Dynamic contrast enhanced MRI imaging may just be that something.
I initially came across this work as a poster at ECTRIMS 2016!
I initially came across this work as a poster at ECTRIMS 2016!
What exactly are they measuring? Ki is a measure of influx of contrast agent into the brain, in this instance into the normal appearing white matter (NAWM; the white matter region of the brain). They have previously demonstrated that this reading correlates with biological markers of immune cells entering into the cerebrospinal fluid via the blood brain barrier (BBB). And, not surprisingly it is a good predictor of conversion to MS from the initial clinical event.
It is a prospective study where things are measured over time rather than going back to the database to see if the information was there or not, and included RRMS cases prior to starting natalizumab or fingolimod treatment. They used NEDA (no evidence of disease activity; clinical relapses and increase in disability as measured by EDSS score and MRI activity) as a markers of treatment success.
"After one year of second-line treatment 12 out of 35 subjects (34%) lost NEDA-3 status. After two years this increased to 15 out of 35 (43%)".
The authors found that single measure of Ki performed at 6 months after initiation of either treatment was predictive loss of NEDA status within the first two years of treatment. But, whether it would be a useful measure in terms of providing long-term prognostic information, since it's simply a surrogate measure of BBB permeability is key. Moreover, there was no correlation between Ki and gadolinium enhancing lesions at baseline. Although, those with one or more gadolinium enhancing lesions tended to have higher ki, they were not significantly different from those with no gadolinium enhancing lesions. What does this mean? ki is not a measure of focal inflammatory activity but possibly of a wider disease process occurring in MS.
Last but not least, the authors did not find any treatment differences between natalizumab and fingolimod in ki measures. Although, these figures were muddied by use of iv steroids and relapses. This may prove to be a problem if the measure is widely adopted in future clinical trials.
Last but not least, the authors did not find any treatment differences between natalizumab and fingolimod in ki measures. Although, these figures were muddied by use of iv steroids and relapses. This may prove to be a problem if the measure is widely adopted in future clinical trials.