Sci Transl Med. 2015 May 13;7(287):287ra74. doi: 10.1126/scitranslmed.aaa8038.
Myelin-reactive T cells have been identified in patients with multiple sclerosis (MS) and healthy subjects with comparable frequencies, but the contribution of these autoreactive T cells to disease pathology remains unknown. A total of 13,324 T cell libraries generated from blood of 23 patients and 22 healthy controls were interrogated for reactivity to myelin antigens. Libraries derived from CCR6+ myelin-reactive T cells from patients with MS exhibited significantly enhanced production of interferon-γ (IFN-γ), interleukin-17 (IL-17), and granulocyte-macrophage colony-stimulating factor (GM-CSF) compared to healthy controls. Single-cell clones isolated by major histocompatibility complex/peptide tetramers from CCR6+ T cell libraries also secreted more proinflammatory cytokines, whereas clones isolated from controls secreted more IL-10. The transcriptomes of myelin-specific CCR6+ T cells from patients with MS were distinct from those derived from healthy controls and, notably, were enriched in T helper cell 17 (TH17)–induced experimental autoimmune encephalitis gene signatures, and gene signatures derived from TH17 cells isolated other human autoimmune diseases. These data, although not causal, imply that functional differences between antigen-specific T cells from MS and healthy controls are fundamental to disease development and support the notion that IL-10 production from myelin-reactive T cells may act to limit disease progression or even pathogenesis.
It has been known for sometime that we all harbour myelin reactive cells whether we have MS or not. Some people use this to say that MS has nothing to do with myelin reactive cells.
However, other people maintain they are functionally different because they are part of the problem and have shown that they have a different activation status. So this study which was part of the key note presentation in ECTRIMS in Boston, which some people said was the "talk of the year" and examines this same question in a different way.
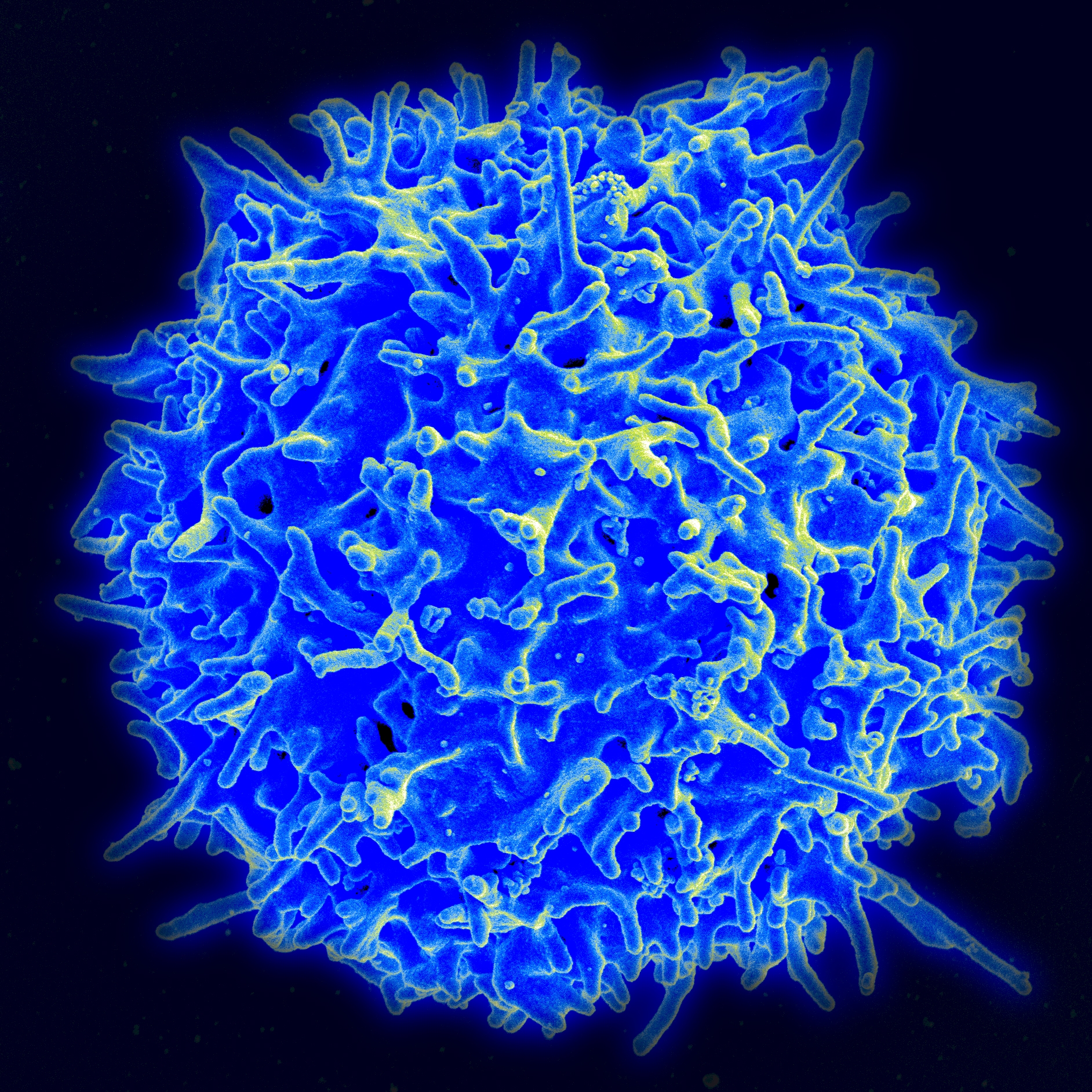
They look at T cells from MS and from healthy people and look at what proteins they are producing by making a library where each book represents a different protein that the cell is making. They look at T cells expressing a chemokine receptor called CCR6 from MS and find that they make more cytokines than from health controls. This suggests that they have been activated....therefore they could be involved in the disease process. They produced gamma interferon and interleukin 17 and GMSCF so supporting the thought that TH1., TH17 may be bad. In the healthy people the cells make IL-10. This cytokine can inhibit some T cell function. The gene expression profile was similar to the genes found in activated T cells in EAE, therefore MS is behaving like the animal model and so they suggest that these cells may be pathogenic. They also then suggest that interleukin 10 may be useful for therapy.

Beautiful work, but it has to be said that it is only layering fine detail on top of what we already know. It suggests that MS is indeed EAE and that the inflammatory response in animals can inform human studies.
Playing devils adovocate one could say that damage during MS releases myelin and we know that it gets out of the brain and into the blood and even peptides have been found in urine, so is it surprising that myelin reactive cells display some activation status that is different from healthy people?
As for interleukin 10. We already know that in EAE that it can inhibit Th1/Th17 responsive T cells....however it is also a B cell differentiation stimulus and can do different things in EAE depending on when and where it is produced and a trial in MS failed.
