Will the anti-B-cell therapies supplant alemtuzumab and natalizumab in MS? #MSBlog #MSResearch
"Although neuromyelitis optica (NMO) is a different disease to MS it is one of the disease that mimics MS; NMOers are frequently misdiagnosed as being MS. This is a problem as most of the DMTs licensed for treating MS make NMO worse. Therefore, it is reassuring to have a treatment strategy that works for both MS and NMO."
"Rituximab is a B cell depleting agent that works in MS. The phase 2 results were spectacular and shifted the paradigm in MS. The anecdotal experience from the off-label use of rituximab in MS has confirmed this; I have personally used rituximab in a handful of cases and have been very impressed with its ability to switch-off disease activity."
"Due to complex, scientific and business, reasons Genentech-Roche decided against taking rituximab forward in MS. Instead they decided to develop the follow-on compound ocrelizumab. This latter decision will delay the access of an anti-CD20 therapy for MSers by about 4 years. At the time Genentech-Roche made the decision not to develop rituximab and to go with ocrelizumab a lot of us felt this was unacceptable, because it would be denying or delaying MSers access to a very effective therapy. Despite our protests the decision was made and the ocrelizumab program is now quite advanced. There are currently three phase 3 ocrelizumab studies running (two in RRMS and one in PPMS) that are due to report in late 2015 and early 2016. The question is not about whether or not ocrelizumab will be effective or not, but rather about safety. There is little doubt that ocrelizumab will be a highly effective DMT. Will it be safe? The rheumatoid arthritis (RA) and systemic lupus erythematosis (SLE) ocrelizumab development programmes were halted due to safety concerns. Whether or not the same safety issues will arise in MS is yet to be ascertained. I suspect not as MSers are generally much healthier than people with severe RA and SLE. Ocrelizumab will also be an induction therapy and will be given every 6 months for at least 2 years. What is not known is how often redosing will be needed after completing the first 2 years of treatment. The phase 2 extension results presented at the AAN, by Prof. Hauser and suggest that the treatment effects may last at least 18 months, and may be longer, after the last dose. What this NMO study below provides is a framework for developing a redosing schedule based on the recovery of peripheral B cells counts."
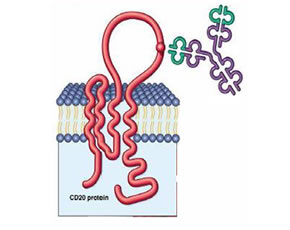
"Why the paradigm shift? Anti-CD20 therapies target B cells by depleting them from the peripheral blood and to some extent from the peripheral tissues. What nobody expected was for these therapies to be so effective in MS; MS was always considered to be a T-cell mediated disease. B cells are the immune cells that make antibodies and are also involved in other immune functions. The B cell is also the niche where EBV resides once you become infected with the virus. Therefore anti-CD20 therapies are also anti-EBV drugs; in fact rituximab is the only licensed drug to treat EBVassociated diseases. In short anti-CD20 therapies have multiple potential modes of action. The onset of action of anti-CD20 therapies is too quick, i.e. within weeks of dosing, for them to be having their effect via antibody production. Most of feel the mode of action anti-CD20 therapies in MS must be related to its impact on the other immunological functions or against EBV. Because of the latter I have branded the anti-CD20 therapies as being anti-EBV and challenge people in the field to prove that these drugs are not working via EBV. Unfortunately, to date no one has risen to the challenge."
"Apart from ocrelizumab (Roche) GSK is currently developing ofatumumab for MS; both drugs target CD20 on the surface of B-cells. Another target is CD19, which to me is even more appealing than CD20 as it is expressed on a larger number of cells including plasmablasts. At present we are recruiting RRMSers for a trial of MEDI-551, which is an antibody that depletes B cells via the CD19 receptor (http://multiple-sclerosis-research.blogspot.co.uk/2012/11/anti-cd19-and-multiple-sclerosis.html)."
"I am of the opinion that if no major safety signals emerge with the anti-CD20 and anti-CD19 therapies that these classes of drugs will supplant the other monoclonal antibodies. The good news is that PPMSers will get an answer with regard to whether or not this class of drug is effective in PPMS at the same time as RRMSers. Who said we are ignoring PPMS?"
Kim et al. A 5-Year Follow-up of Rituximab Treatment in Patients With Neuromyelitis Optica Spectrum Disorder. JAMA Neurol. 2013 Jul 29.
IMPORTANCE: A previous 2-year analysis of repeated rituximab treatment in NMOers (people with neuromyelitis optica (NMO)) revealed significant improvements in relapse rates and disability. This paper reports the findings from the longest follow-up of rituximab treatment in NMO, which provide reassurance regarding the long-term efficacy and safety of rituximab in NMO.
OBJECTIVE: To report the results of rituximab treatment in NMOers with relapsing NMO or NMO spectrum disorder (NMOSD) for a median of 60 months.
IMPORTANCE: A previous 2-year analysis of repeated rituximab treatment in NMOers (people with neuromyelitis optica (NMO)) revealed significant improvements in relapse rates and disability. This paper reports the findings from the longest follow-up of rituximab treatment in NMO, which provide reassurance regarding the long-term efficacy and safety of rituximab in NMO.
OBJECTIVE: To report the results of rituximab treatment in NMOers with relapsing NMO or NMO spectrum disorder (NMOSD) for a median of 60 months.
DESIGN, SETTING, AND PARTICIPANTS: Retrospective case series in an institutional referral center for MS, including 30 NMOers or NMOSDers.
INTERVENTIONS: After induction therapy, a single infusion of rituximab (375 mg/m2) as maintenance therapy was administered whenever the frequency of re-emerging CD27+ memory B cells in peripheral blood mononuclear cells, as measured with flow cytometry, exceeded 0.05% in the first 2 years and 0.1% thereafter.
INTERVENTIONS: After induction therapy, a single infusion of rituximab (375 mg/m2) as maintenance therapy was administered whenever the frequency of re-emerging CD27+ memory B cells in peripheral blood mononuclear cells, as measured with flow cytometry, exceeded 0.05% in the first 2 years and 0.1% thereafter.
MAIN OUTCOMES AND MEASURES: Annualized relapse rate (ARR), disability (Expanded Disability Status Scale score), change in anti-aquaporin 4 antibody, and safety of rituximab treatment.
RESULTS: Of 30 NMOers, 26 (87%) exhibited a marked reduction in ARR over 5 years (mean [SD] pretreatment vs posttreatment ARR, 2.4 [1.5] vs 0.3 [1.0]). Eighteen NMOers (60%) became relapse free after rituximab treatment. In 28 NMOers (93%), the disability was either improved or stabilized after rituximab treatment. No serious adverse events leading to discontinuation were observed during follow-up.
CONCLUSIONS AND RELEVANCE: Repeated treatment with rituximab in NMOers over a 5-period, using an individualized dosing schedule according to the frequency of re-emerging CD27+ memory B cells, leads to a sustained clinical response with no new adverse events.
CONCLUSIONS AND RELEVANCE: Repeated treatment with rituximab in NMOers over a 5-period, using an individualized dosing schedule according to the frequency of re-emerging CD27+ memory B cells, leads to a sustained clinical response with no new adverse events.
CoI: multiple
Other posts of interest:
14 Nov 2012
In response to a query re anti-CD19 treatment. Unfortunately, you can't access anti-CD19 treatment at present it is not a licensed therapy. However, we are doing a clinical trial of this agent so if you are interested you can ...
30 Jul 2013
BACKGROUND:Rituximab is an anti-CD20 monoclonal antibody approved for non Hodgkin lymphoma and rheumatoid arthritis. It is being considered for the treatment of MS. OBJECTIVES:To evaluate the efficacy and safety ...
04 Dec 2012
"In response to a comment regarding the safety of rituximab and ocrelizumab in MS. This poster was presented at ECTRIMS. This is very reassuring in that the anti-CD20 look as if they will be in the upper zone of efficacy and if ...
11 Nov 2012
Rituximab, a monoclonal antibody that depletes B cells by targeting the CD20 molecule, has been shown to effectively reduce disease activity in MSers with relapsing MS as a single agent. Our investigator-initiated phase II ...
04 May 2012
Then look in MSers and find that some B cells are producing more IL-6 and this excessive production of IL-6 is lost in B cells from rituzimab-treated individuals. This suggests that rituximab is killing the IL-6 producing B cells.
29 Jun 2011
In this observational study the investigators present clinical and spinal fluid findings in 3 patients with SPMS who were treated with rituximab, a drug that target the B-cell or the cell that produces antibodies, for at least 15 ...
08 Jun 2011
Rituximab is a monoclonal antibody that targets a surface protein on B cells called CD20. There is good phase 2 data on its effectiveness when given intravenously (i.e. via a peripheral vein) in RRMS and a subgroup of PPMS ...
13 Apr 2013
Reduced antibody formation after influenza vaccination in patients with neuromyelitis optica spectrum disorder treated with rituximab. Eur J Neurol. 2013 Mar 22. doi: 10.1111/ene.12132. [Epub ahead of print] BACKGROUND ...
04 Jun 2011
In the Rituximab study time to confirmed progression between Rituximab and placebo treated groups was not significant. However, subgroup analyses suggest selective B-cell depletion may affect disease progression in ...
06 Nov 2011
Anonymous Friday, November 25, 2011 10:38:00 am. Is Ocrelizumab a new product? I thought it is perhaps Rituximab with a new name. If it is a new product, then it will come dearly so for patients/payers-will it Gavin? Reply ...
16 Oct 2010
First anonymous- They both have the same targets, i.e. both are anti-CD20 monoclonal antibodies (MAb). However, Rituximab is a chimeric MAb (fusion with mouse protein) whereas Ocrelizumab is is humanised MAb. Making ...